by Dr. Jennifer Welt, PT, DPT
What is Meniere’s Disease?
Meniere’s disease is a rare and generally chronic disorder of the inner ear. It causes recurring episodes of dizziness, ringing in the ears (tinnitus), a feeling of pressure or fullness in the ears, and fluctuating or progressive hearing loss. Episodes of symptoms, or “attacks,” tend to be spontaneous and last several minutes to hours and involve dizziness, imbalance, sensitivity to visual stimuli, nausea, and/or vomiting. Symptoms may be positional after the initial attack. These attacks may occur in clusters, and some people might even be symptom free between them. Symptoms, intensity and frequency of attacks, and presence of impairments between attacks, vary from person to person and from attack to attack. Since there is no consistency, people with Meniere’s disease are often burdened with frustration, anxiety, and depression. As the disease progresses, permanent low- and high-frequency hearing loss and constant feeling of imbalance may occur due to hair cell damage and mechanical changes within the inner ear organs responsible for hearing and balance.
What causes Meniere’s disease?
The exact cause of Meniere’s disease is not known. It has been theorized that the fluid in the inner ear builds up and thickens, causing increased pressure within the inner ear. This could be due to reduced drainage, increased fluid production and accumulation, or an autoimmune disorder. It has also been discussed that Meniere’s and Migraines might be related, having many of the same symptoms and overlapping non-drug treatment options. Viral infections of the inner ear, circulatory problems, head injury, allergies, and hereditary predisposition have also been considered in the literature.
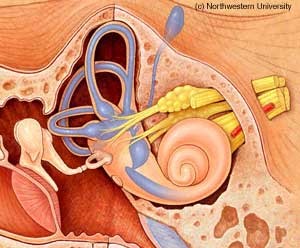
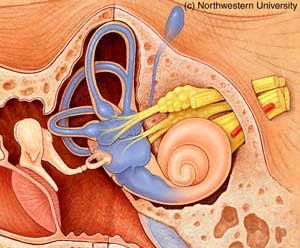
These figures depict the inner ear structures and the fluid inside them. The picture on the left is a normal inner ear. The picture on the right demonstrates inner ear swelling and dilation typical of Meniere’s disease.
How is Meniere’s disease diagnosed?
In addition to a detailed history of symptoms and complaints and exclusion of other possible causes, there are several tests that may help to diagnose Meniere’s disease. These include hearing tests, an ENG (electronystagmography) test, a VEMP (vestibular evoked myogenic potential) test, rotary chair test, posturography, several blood tests, tympanometry, and an MRI of the head.
How can Meniere’s disease be managed?
Currently there is no known cure for Meniere’s disease, but symptoms and attacks may be managed conservatively for most people. During an acute attack, you should move slowly, lay down and focus your eyes on a stationary object, and avoid eating or drinking until severe symptoms subside. Medications may be prescribed for use during acute attacks such as antiemetics and vestibular suppressants.
To cope with the disease and reduce the intensity and frequency of attacks, simple lifestyle changes may be effective. You should maintain a low-sodium (2000 mg) and well-balanced diet, reduce caffeine and alcohol intake, get enough sleep, partake in regular exercise, practice safe stress management, and take medications as prescribed. Medications may be useful for between attacks, such as diuretics, steroids, anti-anxiety, anti-depressant, and vestibular suppressant medications. In severe cases, and when conservative options are not sufficient, further and more radical medical management such as surgery may be required to manage Meniere’s disease.
What should I expect in Physical Therapy?
Physical therapy can be a useful tool to help manage the symptoms associated with Meniere’s disease. Therapists can coach patients through the lifestyle changes mentioned above and can give recommendations for safe mobility during and between attacks. Also, physical therapy can help with dizziness, imbalance, walking abnormalities, and motion sickness that you may experience between attacks and/or after surgical-management interventions.
If you are having difficulty with dizziness or pain, contact Capital Area PT in Malta, Saratoga or Queensbury NY.