by Abigail Frateschi, SPT
 text test | 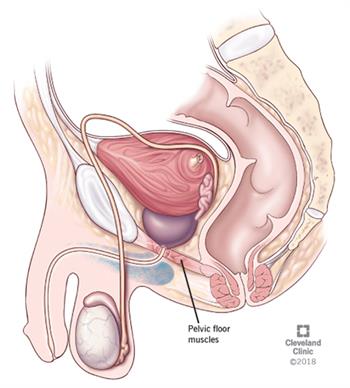 |
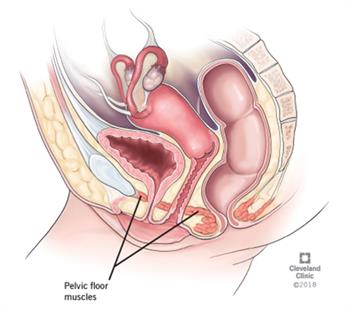
| Image courtesy of the Cleveland Clinic https://my.clevelandclinic.org/health/diseases/14459-pelvic-floor-dysfunction | |
Pelvic Floor Muscle Assessment & Treatments
What is the pelvic floor?
The pelvic floor is a sling like structure that spans from the front of the pelvis to the coccyx and sacrum. It is made up of ligaments, fascia, nerves, and muscles including the levator ani, coccygeus, obturator internus, and piriformis. The pelvic floor functions to support to the pelvic organs, allow for bowel and bladder function, allow for sexual function, and provide stabilization to the spine. Additional muscles, such as the diaphragm, transverse abdominis, and multifidus, also work in conjunction with the pelvic floor to contribute to adequate functioning. Due to the complex nature of the pelvic floor, a great deal of coordination and relaxation is necessary.
What is pelvic floor muscle dysfunction?
Pelvic floor muscle dysfunction describes the complications that result when the pelvic floor musculature is overactive (hypertonic) or underactive (hypotonic). Motor planning deficits, or issues with sequencing pelvic floor contractions with other muscles may also result in PFMD.
A hypertonic or hypotonic pelvic floor can occur for a variety of reasons including but not limited to: injury to the pelvic floor, dysfunction of the lower spine, pelvis, or hips, chronic constipation, obesity, and hormonal changes. Patients with PFMD typically report symptoms of urinary or fecal incontinence, chronic pelvic pain, or low back pain. They may also report history of pelvic organ prolapse or inflammatory pain disorder such as interstitial cystitis or painful bladder syndrome.
Physical Therapy and Pelvic Floor Muscle Dysfunction
Through a thorough history review, screenings, and physical exams a physical therapist can identify impairments contributing to an individual’s PFMD. Interventions generally consist of manual techniques, therapeutic exercise, and motor learning programs to either strengthen, lengthen, or improve coordination of the pelvic floor muscles.
Manual techniques may include:
- Mobilization
- Myofascial release
- Trigger point release
- Joint manipulation
- Visceral mobilization
Therapeutic exercise may include:
- Pelvic floor muscle training
- Strengthening of spinal stabilizers
- Diaphragmatic breathing
- Hip rotation and adduction strengthening
Motor learning interventions may include:
- Education on proper pelvic floor muscle contraction
- Co-activation of pelvic floor muscle contraction with the diaphragm and other spinal stabilizing muscles
Fr more information on physical therapy and Pelvic Floor Muscle Dysfunction and the role that PT can play in treatment, contact us at 518-289-5242 (Malta) or 518-289-5242 (Queensbury).





